FHIR Your Workflow: Future-Proofing HEDIS and Risk Adjustment for Provider Success
07 Aug

In value-based care, HEDIS® performance and accurate risk adjustment are more than quality metrics—they’re critical drivers of reimbursement and provider reputation. Yet many organizations still rely on manual chart reviews, batch extracts, and disconnected data sources to compile their HEDIS submissions and risk profiles. The result? Missed measures, under-captured diagnoses, and avoidable revenue leakage.
Fast Healthcare Interoperability Resources (FHIR) offers a modern, standardized foundation to future-proof HEDIS and risk-adjustment workflows. By exposing all quality- and risk-relevant data, such as diagnoses, encounters, labs, medications, and social-need screenings, as FHIR resources, organizations gain real-time, vendor-agnostic access to the information they need. Embedded automation and analytics then surface missing codes, flag documentation gaps, and close care gaps continuously—without disrupting clinician workflows.
1. Why HEDIS & Risk Adjustment Are Falling Behind
- Manual Chart Chases: Quality teams spend weeks requesting records, retrieving external charts, and manually abstracting data, just to meet submission deadlines.
- Fragmented Data: Critical elements live in disparate systems: EHR modules, care-management platforms, lab systems, and community-partner records.
- Lagging Visibility: Batch data loads and retrospective claims analyses reveal gaps too late to remediate before pay-for-performance deadlines.
These processes drive inefficiency, inflate labor costs, and leave revenue on the table when diagnosis codes or measure data go unreported.
2. FHIR Fundamentals: A Single, Real-Time Data Stream
FHIR is both a data model and an API specification designed for the modern web:
- Resources: Everything from patient diagnoses (Condition), lab results (Observation), encounters (Encounter), to care-plan reviews (QuestionnaireResponse) maps to a standardized FHIR resource.
- APIs: Secure RESTful endpoints enable on-demand queries (GET) or event-driven updates via Subscriptions, eliminating the need for bespoke interfaces or overnight batch extracts.
- Bulk Data: The $export operation retrieves large cohorts of resources in bulk, accelerating population-level analyses.
By consolidating all quality and risk elements on a FHIR server, organizations create a single source of truth that’s always current and fully auditable.
3. Mapping HEDIS Measures to FHIR Resources
Digital HEDIS measures leverage Clinical Quality Language (CQL) running against FHIR data:
- Denominator Identification: EHR encounters (Encounter), patient demographics (Patient), and care settings define the initial population.
- Numerator Criteria: Lab results (Observation for A1c, LDL), procedural data (Procedure for screenings), and documented interventions (Condition for hypertension control) feed CQL logic.
- Exclusions & Exceptions: FHIR accurately represents allergies, medical exceptions, and patient refusals via Condition and Procedure resources.
NCQA’s shift to machine-readable measures in CQL on FHIR has slashed interpretation errors and standardized HEDIS implementations nationwide.
4. Automating Gap Closure with Subscriptions & Analytics
Once HEDIS-relevant data flows in real time, automation can maintain measure compliance continuously:
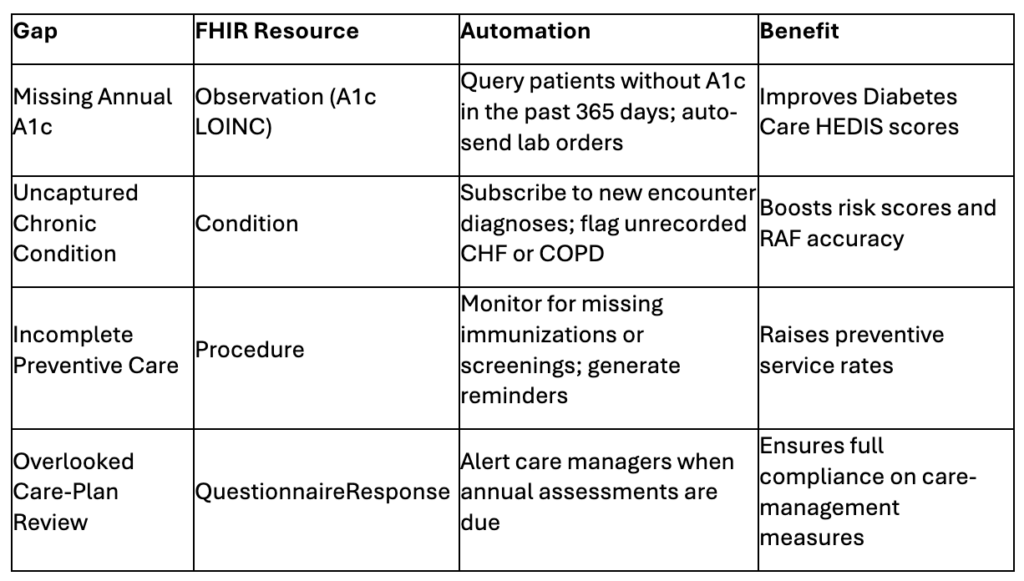
These workflows can be embedded directly in EHR task lists or care-team dashboards—so clinicians and quality staff never leave their primary systems.
5. Bulk Data & Continuous Quality Surveillance
For population-level oversight, the FHIR Bulk Data interface powers nightly or intra-day exports of all quality and risk resources. Organizations can then:
- Visualize Trends: Real-time dashboards track HEDIS measure attainment and RAF score distributions by provider, site, or patient segment.
- Benchmark Performance: Compare against historical baselines or peer cohorts to identify outlier performance.
- Model Revenue Impact: Predict how closing specific gaps boosts overall HEDIS scores and value-based reimbursements.
Moving from annual, scramble-driven audits to continuous quality improvement cycles fosters incremental gains and protects revenue year-round.
6. Data Quality at the Source
“Data quality is contextual,” says NCQA’s Ed Yurcisin. If data is reliable for HEDIS, it’s reliable for prior authorization, public health, and AI analytics. FHIR’s standardized validation rules, such as conformance checks, terminology services, and automated EHR validations, ensure the data feeding your HEDIS and risk pipelines is clean, consistent, and audit-ready.
7. The Business Case: Quality Scores, Risk Scores, and Revenue Integrity
By embedding FHIR-enabled workflows, organizations realize:
- Higher HEDIS Scores: Automated gap closure leads to sustained improvements across diabetes, hypertension, preventive care, and care-management measures.
- Optimized Risk Adjustment: Comprehensive diagnosis capture maximizes Risk Adjustment Factor (RAF) scores, securing full value-based reimbursements and preventing revenue leakage.
- Operational Efficiency: Quality teams reclaim hundreds of chart-review hours annually, while clinicians document care normally, confident that FHIR integrations handle the reporting logic.
- Continuous Quality Improvement: Real-time insights enable rapid Plan-Do-Check-Act (PDCA) cycles, driving incremental performance gains without year-end panics.
8. Why Aigilx Health?
Building and maintaining FHIR-driven HEDIS and risk workflows demands deep interoperability and analytics expertise. Aigilx Health delivers:
- Enterprise-Scale FHIR Servers: Processing millions of clinical, lab, and social-needs transactions daily with enterprise-grade security and compliance.
- Interoperability Leadership: Pioneering HIE-scale integrations that unify EHRs, care-management platforms, and community data.
- Analytics & Automation Mastery: Two decades of refining predictive and quality-measure algorithms, transforming raw data into actionable insights.
- End-to-End Partnership: From FHIR profile mapping and CQL measure implementation to subscription configuration, dashboarding, and clinician enablement.
Partner with Aigilx Health to future-proof your HEDIS and risk-adjustment processes. Transform manual chart chases into continuous, FHIR-powered workflows, boosting quality scores, safeguarding revenue, and freeing your teams to focus on patient care.
Go Beyond FHIR—With Free Tools That Support Your Entire Quality Strategy
At Aigilx Health, we don’t just provide compliance-ready FHIR workflows—we empower providers with free, robust tools for quality checks and validation. These tools aren’t limited to just FHIR, HL7, or C-CDA—they’re designed to support broader data quality efforts across your healthcare ecosystem. Whether you’re preparing for HEDIS, risk adjustment, or simply ensuring clean, interoperable data, our tools help future-proof your performance and outcomes.
Connect with Aigilx Health to learn how FHIR can revolutionize your quality and risk management in value-based care.
Categories
- 1115 Waiver (8)
- ACO (7)
- AI (2)
- Aigilx Health (2)
- CCBHC (8)
- Control Center (10)
- FHIR Facade (7)
- FHIR Server (14)
- HIE (5)
- Payers (8)
- Providers (11)
- Rapid Fire (9)

Aigilx health specializes in developing Interoperability solutions to create a healthcare ecosystem and aids in the delivery of efficient, patient-centric and population-focused healthcare.
